If you receive a blue MassHealth envelope in the mail this year, it’s the first sign that you need to reapply for the state’s Medicaid program.
MassHealth is expected to re-check the eligibility of 2.3 million Massachusetts residents this year. They began the redetermination process in April and will continue until March 2024. Although it had been an annual process, renewals were put on hold during federal and state public health emergencies related to COVID-19. Those emergencies and the continuous insurance coverage granted during them ended this spring.
If you have MassHealth now, the renewal process will likely affect you, although what you can expect varies from when or if you’ll be asked to reapply, how complicated the reapplication process will be, and what it will mean for your health coverage.
Paula Sipple and Jennifer Ouellette, coordinators in Coastline’s Community Mainstream program, say they are seeing people’s experiences range from automatic renewals to applications that are anywhere from a few to 20-pages long.
Sipple and Ouellette work with Coastline consumers and New Bedford residents over age 60 helping them complete reapplication forms. Collectively, they’ve helped hundreds of people reapply over the years or, if they don’t requalify, referred them to additional assistance finding alternative health insurance.

“Most of the people we see don’t get out of the house very much. They don’t drive,” said Sipple, about visits.
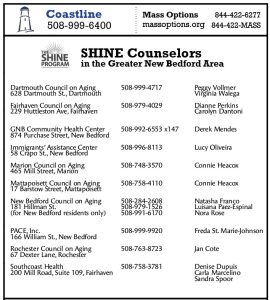
For individuals who don’t meet Coastline criteria, help is also available from the region’s SHINE counselors. The SHINE program provides free health insurance information and counseling to all Massachusetts residents. SHINE counselors can usually be reached through your local council on aging.
Both Sipple and Ouellette recommend seeking help from those familiar with the forms and the reapplications process. There are strict income and asset requirements for qualifying, they say, and knowing which assets count and how they affect your eligibility status is important — particularly for those new to MassHealth.
“Lots of people have only gotten on MassHealth in the last three to four years and never renewed before, so there are probably quite a few people who may be surprised to get a renewal notice,” said Ouellette.
Coastline and SHINE counselors can also help people know which documents and statements they’ll need to complete the application.
Whether you’ve received your reapplication form or expect to soon, it’s important to keep your information up-to-date, said Sipple. MassHealth requires that changes to information such as your name, address, contact information or marital status be updated within 10 days of the change.
Although MassHealth has built in checks to keep as many people from losing health insurance due to renewal complications as possible, it is best to reach out for assistance as soon as you get your form. For those who may no longer qualify, calling will also help you connect with support for signing up for alternative health insurance.
It all comes down to those blue envelopes.
“If you get a blue envelope, you’ll have 45 days to respond and then they’ll send a second notice out,” said Ouellette. “If you don’t get a blue envelope and if they don’t get in touch with you, just keep on going. You’re all set.”
Coastline’s Community Mainstream program can be reached by calling 508-999-6400. See also the list of SHINE professionals and contacts at right.


Recent Comments